Therapie von Blutungs- und Zyklusstörungen
Medikamentöse Behandlung von starken Gebärmutterblutungen
-
General Guidelines
Drug therapy can be very useful for many women with menorrhagia
The use of nonhormonal agents is an appropriate first choice when the menstrual cycle is regular.
- The first options are nonsteroidal anti-inflammatory drugs, with reported reductions in menstrual blood loss of 25% to 35%.
- Tranexamic acid is a drug that enhances blood clotting and is used more in Europe than in the US. It is proving to be very effective, and women might ask their physician if it is available.
Women should feel confident that they understand all of their options and exercise their own treatment preferences.
A general drug treatment regimen for menorrhagia is as follows:
NONHORMONAL AGENTS.
Nonsteroidal Anti-inflammatory Drugs (NSAIDs).
- Nonsteroidal anti-inflammatory drugs (NSAIDs) block prostaglandins (the substances that increase uterine contractions).
- They also have other properties that act against inflammatory factors that may be responsible for heavy menstrual bleeding.
- Studies suggest that they reduce bleeding by 30% to 50% and are the first choice for most women who experience heavy menstrual bleeding.
- Aspirin is the most common NSAID, but there are dozens of others available over the counter or by prescription. Among the most effective NSAIDs for menstrual disorders are ibuprofen, naproxen and mefenamic acid.
- Mefenamic acid has been intensively studied and has been shown to reduce bleeding by 30% to 50%.
- For maximum benefit, they should be taken seven days before a period is expected.
- It should be noted, however, that long-term use of any NSAID can increase the risk for gastrointestinal bleeding and ulcers.
Tranexamic Acid.- Tranexamic acid is a synthetic form of the amino acid lysine and enhances blood clotting.
- It reduces menstrual blood flow by about half.
- It is more effective in reducing blood flow than oral progestins or NSAIDs, but is not as effective as the progestin-releasing IUD (LNG-IUS).
- Women reported a better quality of life with tranexamic acid than with oral progestins.
- Side effects, however, can include headache, nausea, and gastrointestinal distress.
- Tranexamic acid may be a good treatment choice for menorrhagia not caused by fibroids, endometriosis, or other uterine lesions and when hormonal agents are not an option.
- Women with any risk factors for blood clots should not use this agent.
HORMONAL AGENTS.Hormonal agents are useful for women with heavy bleeding who also want to control the menstrual cycle.
- The best choice for women who also want effective birth control is either the combined oral contraceptive pill or a progestin containing intrauterine device.
- The levonorgestrel-releasing intrauterine system, or LNG-IUS (Mirena, FibroPlant) specifically is proving to be a particularly effective treatment for menorrhagia.
- Danazol and the gonadotropin-releasing hormone (GnRH) analogues are highly effective for more severe cases, but their side effects make them suitable only for short-term use. These agents are also useful as pretreatment before procedures used to destroy the uterine lining. Both are effective, but GnRH analogues may be slightly better.
- The first options are nonsteroidal anti-inflammatory drugs, with reported reductions in menstrual blood loss of 25% to 35%.
Hormonelle Behandlungsoptionen
The hormonal agents that can be used for treating dub include
- Combined oral contraceptive pills
- Progestins
- GnRH- analogues
- Danazol
- Others
COMBINATION ORAL CONTRACEPTIVES
Oral contraceptives (OCs), commonly known collectively as „the Pill,“ contain combinations of an estrogen and a progestin (either a natural progesterone or the synthetic form called progestogen).
These agents block production of male hormones and inhibit receptors for estrogen in the uterus.
OCs are often used to regulate periods in women with menstrual disorders, including menorrhagia (heavy bleeding), dysmenorrhea (severe pain), and amenorrhea (absence of periods).
They also protect against ovarian and endometrial cancers .
It is not clear, however, if they are any more effective than NSAIDs in reducing heaving bleeding, but they may still be a good option for women seeking both birth control and relief from menorrhagia.
Combination pills are sold in 21-day or 28-day packs:
- Each pill in the 21-day pack contains the necessary estrogen and progestin.
- The 28-day pack adds seven differently colored „reminder“ pills; they are inactive and do not contain hormones, but help the user maintain her daily routine during seven days between active pill use.
OCs may be taken in cycles that include pills of the same or different strengths.
These are categorized as monophasic (one-phase), biphasic (two-phase), or triphasic (three-phase).
- Monophasic regimen
A 21-day pack uses tablets that are one strength and one colour for 21 days. (A 28-day pack adds seven inactive tablets of a different colour.)
- Biphasic regimen
A 21-day pack consists of tablets of one strength and colour taken for seven or 10 days, then a second tablet with a different strength and colour for the next 11 or 14 days.
- Triphasic regimen
This pack consists of tablets with three different colors and strengths. In the first phase, there are tablets of one color for five to seven days; for phase two, a second color and strength tablets is taken for five to seven days; and for phase three, a third color and strength tablet is taken for five to 10 days.
The difference in duration of each phase depends on the brand.
In all cases, women continue to menstruate, but their periods are lighter, shorter, more regular, and less painful than bleeding in women who are not on the pill.
The monophasic regimen is the most studied regimen and at this time is preferred.
Estrogen and progestin each cause different side effects
Uncommon but more dangerous complications of OCs include high blood pressure and deep-vein blood clots (thrombosis), which may contribute to heart attacks or strokes.
It should be noted that a long-term study of 46,000 British women found no difference in mortality rates between women who took OCs and those who did not.
The most serious side effects are due to the estrogen in the combined pill. Women at risk can usually take progestin-only contraceptives.
Other Forms of Combination Contraceptives.
Other methods for delivering contraceptives include skin patches, monthly injections, and vaginal rings. It is not clear, however, if they have any advantages for women with heavy bleeding.
PROGESTINS
- Progestins (either natural progesterone or synthetic progestogen) are used by women who clearly have dysfunctional uterine bleeding caused by unopposed production of estrogen.
- A number of forms are available and have specific advantages and disadvantages.
- In addition to reducing bleeding, another important advantage is that they appear to protect against uterine and ovarian cancers.
- It should be noted that some progestin treatments, such as implants, can cause menorrhagia in the first few months.
- Progestins can be delivered in various forms.
Progestin-Releasing IUDs
- Intrauterine devices (IUDs) that release progestin may be very beneficial for menstrual disorders.
- Specifically, the levonorgestrel-releasing intrauterine system, or LNG-IUS (Mirena, FibroPlant) is proving to have important effects on menstrual disorders, regardless of its contraceptive effects.
- The LNG-IUS is now considered to be one of the best options for treating menorrhagia.
- It also reduces pain and may help prevent endometriosis.
- Progestin released by an IUD mainly affects the uterus and cervix and so it causes fewer widespread side effects than the progestin pills do.
- It should be noted that the other major IUD–the Copper T–may increase bleeding.
- Irregular break-through bleeding can occur for the first six months, but afterward 80% to 90% reduction in blood loss has been reported.
- It is well tolerated. It may even be appropriate and protective for women with uterine fibroids, but studies to date suggest it is less effective in reducing menstrual bleeding from fibroids than from other causes.
Oral Progestins.
- Oral progestins include medroxyprogesterone, norethindrone acetate, and norgestrel
- Taking such agents for 21 days is effective in reducing bleeding.
- Oral progestins, however, have unpleasant psychological and physical side effects such as bloating, depression, moodiness, and breakthrough bleeding.
- Natural progestins (called progesterone) may be helpful.
- A natural oral form of finely ground (micronized) progesterone is also available and has fewer side effects.
Injections (e.g., Depo-Provera).
- Depo-Provera uses a progestin called medroxyprogesterone.
- Unlike users of the implants, most users of Depo-Provera stop menstruating altogether after a year.
- It may be beneficial for women with heavy bleeding, severe cramps, or both.
- Women who eventually want to have children should be aware that Depo-Provera can cause persistent infertility for up to 22 months after the last injection, although the average is 10 months.
- Weight gain can be a problem, particularly in women who are already overweight.
GNRH AGONISTS
- Gonadotropin releasing hormone (GnRH) blocks the release of the reproductive hormones LH (luteinizing hormone) and FSH (follicular-stimulating hormone).
- As a result, the ovaries stop ovulating and no longer produce estrogen.
- GnRH agonists include goserelin (Zoladex), buserelin, a monthly injection of leuprolide (depot Lupron), and a nasal spray, Nafarelin (Synarel).
- Such agents may be used to alone or in combination for procedures used to destroy the uterine lining.
- They are not generally suitable for long-term use.
- Commonly reported side effects (which can be severe in some women) include menopausal-like symptoms that include hot flashes, night sweats, changes in the vagina, weight change, and depression.
- They may be more intense with leuprolide and persist after the drug has been stopped.
- The most important concern is possible osteoporosis from estrogen loss. Women ordinarily should not take them for more than six months.
DANAZOL
- Danazol (Danocrine) is a synthetic substance that resembles a male hormone.
- It suppresses estrogen, and therefore menstruation, and is used (sometimes in combination with an oral contraceptive), to help prevent heavy bleeding.
- It is not suitable for long-term use.
- Adverse side effects include facial hair, deepening of the voice, weight gain, acne, and dandruff.
- It may also increase the risk for unhealthy cholesterol levels.
- Pregnant women or those trying to become pregnant should not take this drug because it may cause birth defects.
AGENTS USED FOR WOMEN WITH VON WILLEBRAND DISEASE AND OTHER BLEEDING DISORDERS
Desmopressin.
- Desmopressin is a drug that stimulates the release of blood factors that are particularly important for women with certain bleeding disorders, especially von Willebrand disease.
- High doses of a nasal spray containing desmopressin acetate, or DDAVP (Stimate) have reduced menorrhagia in women with bleeding disorders, including von Willebrand disease and mild hemophilia.
- Side effects are mild to moderate. They include headache, nausea, and weakness.
Tranexamic acid.
- Tranexamic acid is also useful for treating bleeding disorders.
- This is a synthetic form of the amino acid lysine and enhances blood clotting. (This agent is discussed under Nonhormonal Agents.)
Operationsmöglichkeiten bei starken Gebärmutterblutungen
Choosing Between Surgery and Medical Treatments
Women with DUB now have surgical and medical options available to them.
Surgical procedures include
- endometrial resection
- endometrial ablation,
- hysterectomy.
Choosing Between Endometrial Resection or Ablation
In either standard endometrial resection or ablation, the entire lining of the uterus (the endometrium) is removed or destroyed.
The standard endometrial ablation and resection techniques are equally effective in reducing bleeding. In general, either one reduces bleeding by about half. At least 90% of women find either procedure acceptable and about three-quarters are totally or generally satisfied with the treatment. Only about 15% of women require a hysterectomy later on. Since no procedure has any particular advantage, a woman’s best option may be to select the procedure based on their surgeon’s skill and experience with it.
Newer second-generation endometrial ablation approaches that compare favorably to the standard techniques and are less invasive are being used or investigated.
Hormonal Pretreatment.
The hormonal agents GnRH analogs used before the procedures help to prepare the uterus by thinning the lining. Evidence now strongly supports their use for improving operating conditions and at least short-term outcome.
Complications of Endometrial Ablation or Resection Procedures.
Complications from either procedure may include perforation of the uterus, injury to the intestine, hemorrhage, or infection.
In standard resection and ablation, the uterine cavity is expanded by filling it with fluid. In rare instances, excess glycine from the fluid instilled in the uterus builds up in the bloodstream and causes an abnormal drop in sodium levels. This can be a serious event resulting in mental confusion, convulsions, and very rarely, death. General anesthesia may pose a lower risk for this complication than local. Some of the newer ablation procedures do not require fluid instillation.
ENDOMETRIAL RESECTION
Resection procedures benefit those women who have very heavy menstrual bleeding but do not have any other underlying uterine problems, such as polyps, hyperplasia of the endometrium, or cancer.
Resection also seems to have a higher success rate in reducing bleeding and relieving pain in older women than younger women.
Resection procedures typically involve the following:
- The patients are given a local or general anesthesia.
- The surgeon dilates (widens) the cervix and fills the uterine cavity with fluid to improve visualization.
- The surgeon then removes the uterine lining.
STANDARD ENDOMETRIAL ABLATION WITH HYSTEROSCOPY
Endometrial ablation involves the destruction of the uterine lining using a number of approaches that include heat, electricity, laser energy, and other methods.
The standard ablation approach uses hysteroscopy to allow the physician to view the uterus.
A typical procedure uses the following approach:
- The physician uses hysteroscopy to view the uterine cavity. This is a fiber optic light source inside a long flexible or rigid tube, which is inserted into the uterus in order to view the cavity. The image of the uterine cavity is transmitted by camera lenses to a video screen.
- The uterine cavity is filled with fluid for better visualization. A special substance such as glycine, sorbitol, or mannitol may be added to the fluid so that it does not conduct electricity. This process prevents accidental burns.
- With ablation, uterine tissue is usually vaporized using a thin powerful laser beam or high electric voltage. One ablation technique, known as electrocautery with roller ball diathermy, uses a device that looks like a tiny steamroller. This device applies heat and destroys endometrial tissue as it rolls across the uterine lining.
- The procedure typically takes 15 to 45 minutes. Although a general anesthetic is usually required, the patient can go home the same day.
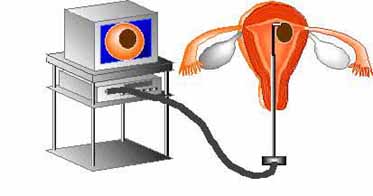
- It takes about three months to determine whether the procedure has been effective. There should be a follow-up appointment after the procedure.
- One study revealed 80% of the women were satisfied with ablation; however, this was lower than the 89% satisfaction rate reported by women who had had hysterectomy. About 30% of women who have this procedure still require additional surgeries, including hysterectomies, within five years. The risk is higher in younger women. It should be noted that the risk for complications increases with repeat ablations.
SECOND-GENERATION ENDOMETRIAL ABLATION PROCEDURES
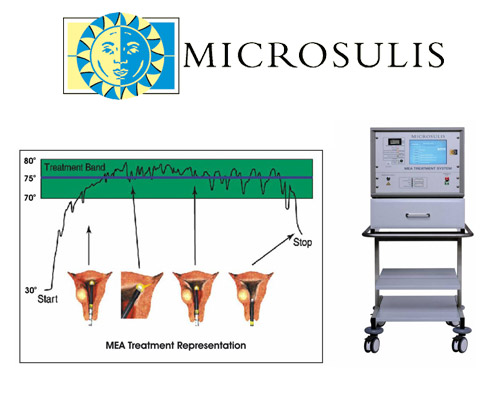
Microwave Endometrial Ablation.
- Microwave endometrial ablation applies very low-power microwaves to the uterus, which limits tissue destruction only to the lining without causing any unnecessary harm to other tissues.
- This device produces effective results by completely destroying the endometrium regardless of uterine shape or size and without the use of a hysteroscope or distension fluids.
- MEA uses high frequency microwave energy to cause rapid but shallow heating of the glandular lining of the uterus causing complete endometrium destruction.
- The microwave frequency chosen for MEA has been specially selected to produce a repeatable and predictable result.
- The microwave energy is delivered by means of an applicator that is gently inserted into the uterus via the cervix.
- When the applicator is inside the uterus, the microwave energy is applied while the applicator is slowly withdrawn with a sweeping movement to ensure that all of the endometrium is treated.
- A link to a computer enables the gynaecologist to monitor and control the treatment temperature throughout the procedure.
- MEA is minimally invasive (involving no incisions of the skin) and is a quick procedure (typical treatment time is 3 to 5 minutes) when compared with competitive devices.
- The high amenorrhoea rates resulting from MEA treatment bear testimony to the effective ablation of the endometrium layer including into the corners of the uterine cavity.
- MEA can treat irregular cavities, cavities with fibroids and cavity length of up to and including 14.5 cm.
- As such, it is the most widely applicable second-generation technique for the patient group.
- It has been extensively tested for over seven years in high quality clinical trials and has an impressive publication record. There have been approximately 12,000 MEA treatments worldwide carried out to date.
Balloon Endometrial Ablation
Balloon ablation is carried out as follows
- A balloon at the tip of a catheter tube is filled with fluid and inflated until it conforms to the walls of the uterus.
- A probe in the balloon heats the fluid to destroy the endometrial lining.
- After eight minutes the fluid is drained out and the balloon is removed.
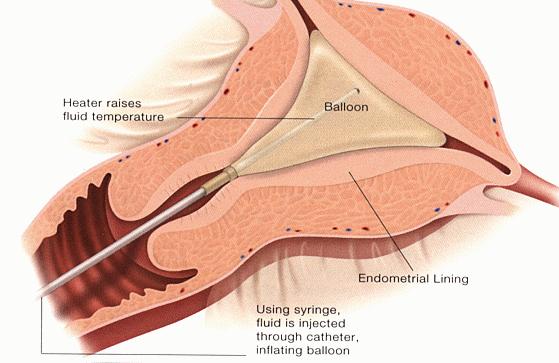
- Studies show that bleeding is controlled in 70% to 90% of patients for at least five years.
- It is fast, simple to perform, and comparison studies are suggesting that it is as effective as resection and standard ablation.
- Treatment is less likely to succeed in younger women, when the uterine lining is 4 mm or thicker, and when menstrual bleeding is prolonged.
- Pregnancy is possible if some of the lining is maintained, but generally women should not depend on it to preserve fertility.
Electric Wand Ablation.
- One approach now approved involves inserting a slender wand up through the cervix (the NovaSure System).
- A triangular mesh-like device is the passed through the wand and expands to fit the uterus.
- Electrical energy is passed through it for about 90 seconds and the mesh and wand are then withdrawn.
- As with many other second-generation ablation techniques, it is quick, effective, and does not require pretreatment to expand the uterus.
- In one 2003 study, it achieved significantly lower bleeding rates than balloon ablation.
Freezing (Cryoablation).
- With cryoablation , the uterine tissue is frozen which destroys the lining.
- The procedure takes about 10 minutes to destroy the lining, and it requires no fluid to expand the uterus and little anesthetic.
- Ultrasound is used to guide the procedure so that the surgeon can view the depth of the ablation.
- In one 2003 study, cryoablation was slightly less successful than a standard ablation procedure.
- However, bleeding still declined by 92% with the freezing technique, and quality of life significantly improved.
Hot Saline.
- Another recently approved technique (Hydro-Therm-Ablator (HTA) system) uses hot saline (salt water) to destroy the lining.
- It takes about 10 minutes to do this.
- This is not a „blind“ procedure but uses hysteroscopy so that the surgeon can view the uterus.
Laser Ablation.
- Endometrial laser intrauterine thermotherapy (ELITT) is an ablation technique that does not require either fluid or devices for expanding the uterus or direct contact with the endometrium.
Radiofrequency.
- An interesting investigative technique (Novacept RF Ablation Generator) employs an inflated device that uses radiofrequency to deliver power and evenly destroy uterine tissue.
- A suction device then removes moisture.
HYSTERECTOMY
- Hysterectomy is the surgical removal of the uterus.
- About 600,000 hysterectomies are performed each year in the US, which is the highest rate among any nations with published data on this procedure. By age 60, about a third of American women have had this procedure. The highest hysterectomy rates are in women between ages 40 and 44.
- Heavy bleeding, often from fibroids, is the reason for about two-thirds of all hysterectomies.
- However, in about half of these hysterectomies, no abnormalities are detected to explain the bleeding.
- In its support, hysterectomy, unlike medical treatments and less invasive procedures, cures menorrhagia completely, and women are satisfied with the procedure.
- Less invasive hysterectomy procedures LIKE GASLESS LIFT-LAPAROSCPIC HYSTERECTOMY are also improving recovery rates and increasing satisfaction afterward.
- For Further Details please see under hysterectomy section
